What are disruptive behaviors
Disruptive behaviors or behavioral alterations are very common symptoms in patients suffering from moderate cognitive impairment or dementia. Behavioral or behavioral symptoms are especially significant because they have a decisive influence on the quality of life of the patient and their family members and/or caregivers.
Behavioral symptoms are defined as symptoms of altered perception, thinking, mood or behavior that often occur in patients with dementia. They include varied manifestations such as physical aggression, restlessness, agitation, erratic wandering, hyperactivity, culturally inappropriate behaviors, sexual disinhibition, etc.
Behavioral disorders contribute to premature institutionalization, reduce the quality of life of the patient and caregivers, and, ultimately, reduce the level of functional autonomy of the people who suffer from it. Although they can occur at any time during the disease, they reach their maximum when reaching the most advanced stages.
Management of disruptive behaviors in cognitive impairment/dementia
Behavioral problems like agitation are difficult to treat. Normally, both pharmacological treatment is used, usually using neuroleptics or antipsychotics such as risperidone, combined with non-pharmacological measures, which are the ones we will focus on.
For example, it is very usefulto facilitate walking in environments free of architectural barriers (patios, parks or gardens), reality orientation therapies, using music or artistic therapies, etc. that reduce restlessness and anxiety, improving sleep and rest and reducing agitation.
It is important to not confront the person when aggression and disruptive behaviors appear, create an appropriate circuit and environment so that they can move and act safely, avoid insomnia and nighttime interruptions by preventing daytime naps and reinforcing appropriate behaviors.
Advice for disruptive behavior in older people with cognitive impairment or dementia
The most common disruptive behaviors are aggression, erratic wandering (walking without rest), agitation and delusions.
Some tips to take care of people who suffer from them and be able to face these situations are:
Tips for dealing with Aggression:
- Avoid confrontations and arguments.
- Do not try to reason and avoid conflict. Do not contradict.
- Approach head-on, staying calm and explaining what we are going to do at all times.
- Use good eye contact, avoid threatening gestures and postures that may create confusion.
- Speak lovingly, softly and evaluate the need for physical contact
- Try to calm down the person, focusing their attention on something else, hopefully being pleasant and conveying calm.
- Avoid physical restraint, whenever possible.
Wandering in a person with cognitive impairment:
- Facilitate a circuit around the home,free of architectural barriers and dangers.
- Use security locks to prevent them from leaving the home. Install security devices on windows.
- Maintain soft lighting, light colors in decoration and walls, which convey calm and relaxation.
- Play appropriate, calm background music.
- Eliminate mirrors, abstract elements, avoid loud colors and noises.
- Facilitate the identification of the person with bracelets or badges. There are other options such as GPS locators, watch or keychain.
- Propose activities thatkeep the person entertained and distracted.
What to do when faced with an episode of Agitation:
- Reduce environmental noise, clutter and the number of people.
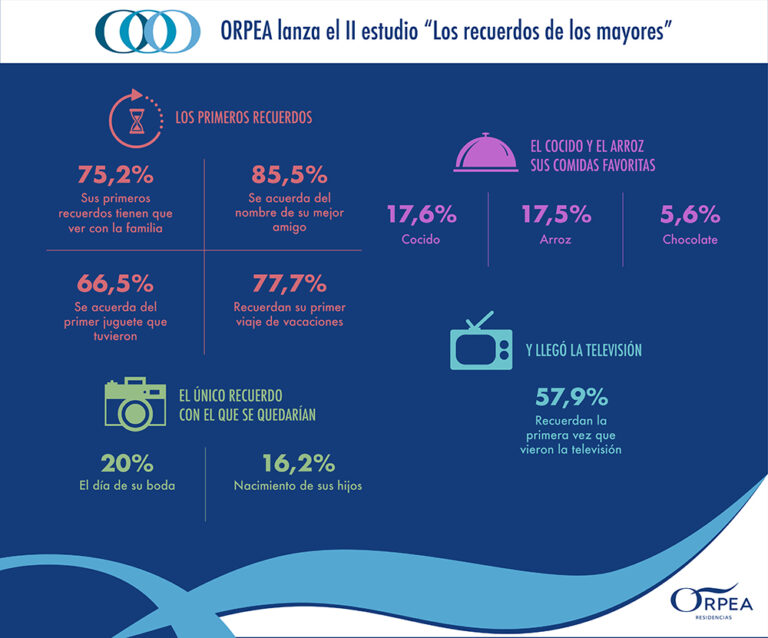
- Maintain a stable environment and fixed routines. Photographs and other familiar objects help create a sense of security and can facilitate pleasant memories.
- Reduce the consumption of caffeine and sweets.
- Use physical contact through gentle caresses, quiet music, reading and walks.
- Speak in a soft, comforting voice. Do not reason when he or she appears agitated.
- Keepdangerous objects out of reach.
- Foster the promotion of autonomy, whenever possible and that the person can take care of their self-care.
How to deal with a person with Delusions:
- Avoid arguments, conflicts and be contrary at the time of delirium.
- Inform other family members and/or caregivers that the accusations and suspicions are part of the illness.
- Use non-verbal means to strengthen the feeling of security, such as a caress or a hug.
- Give security through words, orient to reality, look for things that keep you oriented in space.
- Keep the room well lit to reduce confusing shadows.